Endemic Disease Does Not Necessarily Mean Mild Disease
(Posted on Tuesday, January 18, 2022)
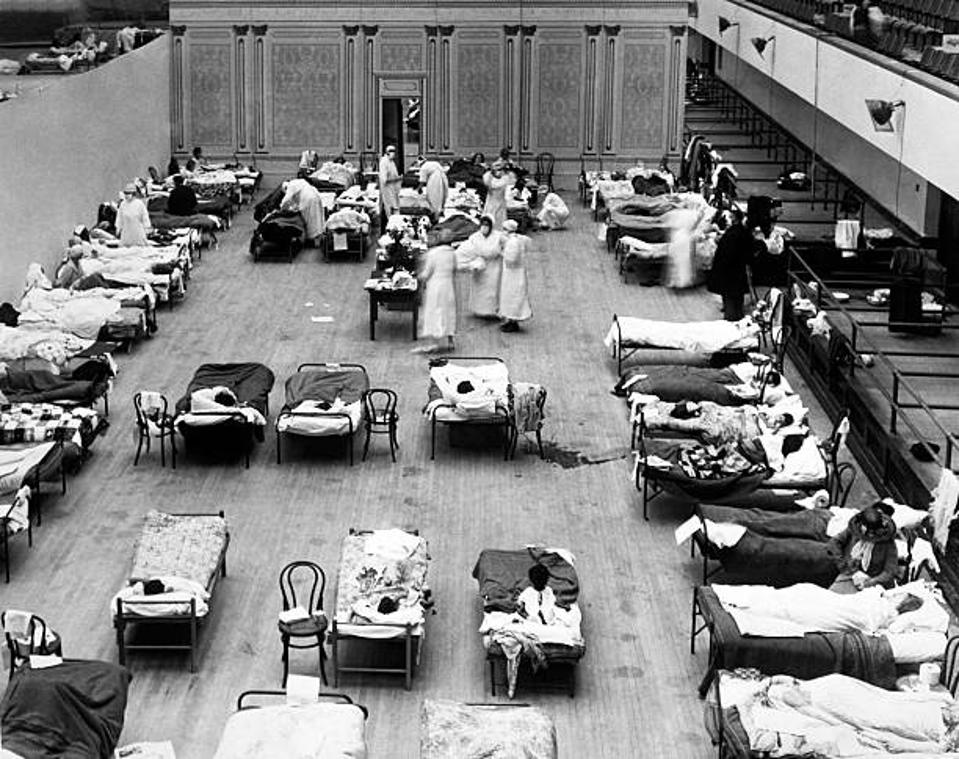
The Oakland Municipal Auditorium is being used as a temporary hospital with volunteer nurses from the American Red Cross tending the sick there during the influenza pandemic of 1918, Oakland, California, 1918. (Photo by Underwood Archives/Getty
GETTY IMAGES
Many are hoping that the Omicron variant signals a transition into the endemic phase of Covid-19 pandemic. But this hope is based on the flawed logic that endemic equals mild, resulting in less severe disease and fewer deaths. This is not always true, diseases like Malaria, are endemic but according to WHO’s latest World malaria report, there were an estimated 241 million malaria cases and 627,000 malaria deaths worldwide in 2020. Many of the greatest plagues of mankind have become endemic such as tuberculosis, cholera, influenza.
Influenza has been endemic for decades but WHO estimates that 290,000 to 650,000 people die of flu-related causes every year worldwide. Many virologists also believe that influenza has the potential to become even more deadly than Covid-19 by undergoing an antigenic shift and transmitting from birds or pigs to humans.
An endemic is a disease outbreak that is consistently present, irrespective of severity. Covid-19 is still a very serious disease with many unknown outcomes. Stable endemic disease is a world away from the unpredictable surges and evolving variants of the current pandemic.
Once again, public health strategies have suffered across the globe at the hands of poor communication and messaging. Early reports of proportionally lower hospitalization rates characterized the Omicron variant as “mild” when hospitalization rates only tell part of the story. Unfortunately, this early perception has proven difficult to shake, with some people even deliberately seeking out infection to “get it over with” or dispensing with mitigation measures.
Once again, public health strategies have suffered across the globe at the hands of poor communication and messaging. Early reports of proportionally lower hospitalization rates characterized the Omicron variant as “mild” when hospitalization rates only tell part of the story. Unfortunately, this early perception has proven difficult to shake, with some people even deliberately seeking out infection to “get it over with” or dispensing with mitigation measures.
With record cases around the world, it has never been more clear that herd immunity is a myth and not a viable strategy when it comes to this virus. Infection with Omicron does not guarantee protection against new variants that are likely to arise.
Omicron infection is not mild for those who are immunocompromised, unvaccinated or have a risk factor for severe Covid-19, which accounts for a significant fraction of the United States population. Unlike the hopeful initial data that emerged from South Africa, hospitalizations in the US have already hit a new pandemic peak.
When Omicron finds a vulnerable host it can still exact SARS-CoV-2’s worst and with the increased transmissibility of this variant, it is finding them fast. The burden on our health systems from Omicron’s surging cases will also affect the standard of care for all healthcare.
Pediatric hospitalizations are the highest they have ever been throughout the pandemic in the US and Europe, with many children too young to be vaccinated and the increased transmissibility of Omicron. We should also be monitoring pediatric hospitalizations for increases in pediatric multisystem inflammatory syndrome (PIMS) as it is not yet known whether Omicron increases the risk of this condition.
There is also much we don’t about Long Covid, beyond the initial infection. A Penn State study from October 2021 found that more than half of the 236 million people who have been diagnosed with Covid-19 worldwide since December 2019 will experience post-Covid symptoms. Those with Long Covid face a challenging road to diagnosis and even then have very few treatments available. Many have found themselves permanently disabled unable to work or care for their families.
Hepatitis C is just one example of another endemic disease that causes significant health issues. WHO estimated that in 2019, approximately 290 000 people died from hepatitis C, mostly from cirrhosis and hepatocellular carcinoma (primary liver cancer). Globally, an estimated 58 million people have chronic hepatitis C virus infection, with about 1.5 million new infections occurring per year.
We can hope for the best, but also we need to prepare for the worst. As pandemic fatigue grows we must still remember to implement the latter part of that maxim. We cannot predict how this virus will change and evolve or what future variants will bring. The only path forward is a Multimodal strategy combining medical defenses such as antiviral drugs and vaccines and public health defenses such as testing, tracing, isolation, ventilation, and masking.

