What Are Our Eyes Telling Us?
(Posted on Wednesday, June 14, 2023)
Originally published on Forbes on 6/9/2023

This story is part of a series on the current progression in Regenerative Medicine. This piece starts a series dedicated to the eye and improvements in restoring vision.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
The field of regenerative medicine is rapidly advancing, offering new hope to individuals suffering from visual disorders. Specifically, there’s a growing potential to restore vision and transform lives with breakthrough treatments.
The human eye, an intricate sensory organ responsible for our ability to perceive the world, has numerous complex structures, such as the cornea, iris, lens, retina, and optic nerve. With these complex structures comes the potential for diseases and disorders that can lead to blindness and visual impairments.
Cataracts, glaucoma, diabetic retinopathy, and age-related macular degeneration are the most common optical conditions affecting millions worldwide. While cataracts result in clouding of the lens leading to blurry vision, glaucoma is caused due to damage in the optic nerve leading to loss of peripheral vision. People with diabetes can also get diabetic retinopathy, a condition that affects the blood vessels in the retina and leads to vision impairment if left untreated.
A recent review took an in-depth look at age-related macular degeneration and regenerative medicine’s role in treating it. Age-related macular degeneration, a leading cause of vision loss among people over 50, affects the center of the retina, leading to blurry or distorted vision.
Age-Related Macular Degeneration and Disease Burden
Age-related Macular Degeneration (AMD), a chronic eye condition, affects 196 million people worldwide as of 2020, and with an expected increase to 288 million by 2040, its prevalence is on the rise. AMD’s impact is extensive, causing a decrease in people’s quality of life, mobility, and independence. In turn, this leads to an increased rate of falls and depression.
This disease has become an important global cause of disease burden and a leading driver of health outcome inequalities, disproportionately affecting countries with low income and low human development index values.
The disease burden in Africa is over twice that of the Americas. Moreover, Asia, which constitutes around 60% of the global population, is projected to carry more than a third of all cases of AMD. Despite considerable progress in treatment, age-related macular degeneration still poses a significant public health challenge.
Classifying Macular Degeneration
Age-related macular degeneration is a medical condition that causes a loss of central vision in the affected eye. This can make daily activities such as reading or driving difficult. It occurs when the cells of the macula, the small area in the center of the retina, begin to deteriorate over time.
The Beckman Initiative for Macular Research proposed a clinical classification system for AMD in 2013, which is now commonly used in research and clinical settings. This classification system requires only clinical examination or color fundus images, making it universally accessible and applicable.
Color fundus images capture intricate details of the fundus. The photos can give insights into the retina, blood vessels, macula, and optic disc. With this, doctors can identify vascular abnormalities, monitor disease progression, and evaluate treatment efficacy. These images are essential in diagnosing and treating AMD.
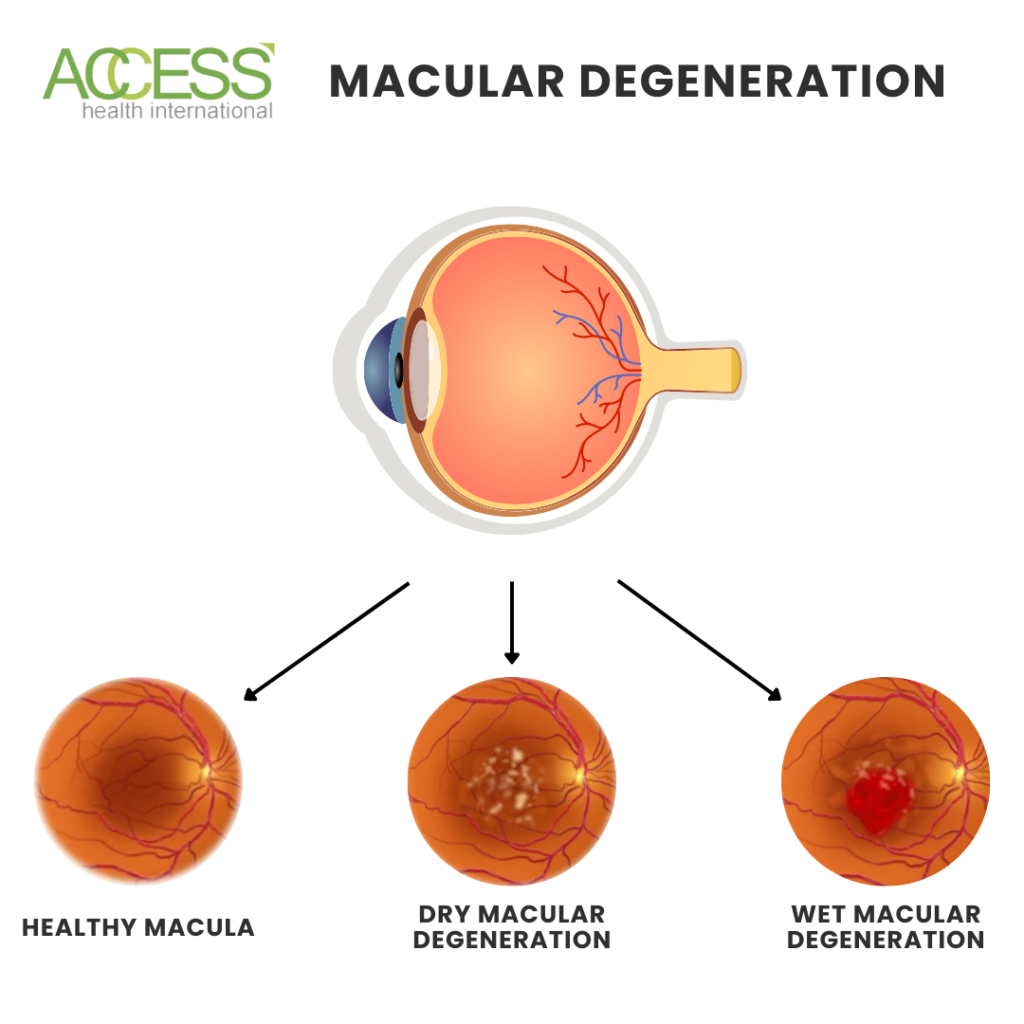
Neovascular AMD, also known as wet macular degeneration, is defined as the presence of neovascularization under the retinal pigment epithelium.
Geographic atrophy, also known as dry macular degeneration, involves the loss of photoreceptors and retinal pigment epithelium and presents as a sharply defined pale area with exposed underlying choroidal blood vessels.
Both types of age-related macular degeneration (AMD) can be asymptomatic in their early stages but may cause night blindness and difficulty adjusting to dim lighting. Early detection and monitoring are crucial for identifying neovascular complications and ensuring timely medical intervention.
What Causes Macular Degeneration?
Age-related macular degeneration is a chronic retinopathy that develops due to oxidative damage to the retina over time. This damage affects various eye structures, including photoreceptors, Bruch’s membrane, choriocapillaris, and the retinal pigment epithelium.
Retinal pigment epithelial (RPE) cells accumulate intracellular debris as we age, mainly lipofuscin or drusen. This buildup leads to oxidative damage and the aggregation of debris into sub-RPE deposits, which manifests as drusen–the hallmark of AMD. This buildup over time is why age is the predominant risk factor for the condition.
Although age is a significant risk factor for macular degeneration, other factors, such as diet and genetics, can also play a role. While lifestyle factors like diet fall under modifiable risk factors, less controllable factors like genetics can’t be changed easily.
Smoking poses the most significant risk of all preventable factors, tripling the probability of developing the condition. Nevertheless, quitting smoking can help reduce this risk. Regular physical activity may offer minor protection, but research has proved it a significant mitigating factor in developing macular degeneration.
Research Leads Us To Future Treatment Insights
Although progress has been made in treating age-related macular degeneration, there are still deficiencies in our understanding of the disease and its management. Currently, research is focused on early intervention trials to slow down or prevent disease progression.
To improve trial accessibility and efficiency, regulatory agency-endorsed primary endpoints play a crucial role. However, thus far, no such metrics for disease progression have been approved, late-stage age-related macular degeneration being a notable exception. Contrast sensitivity, best-corrected visual acuity, and geographic atrophy lesion growth rate remain the only benchmarks recognized by these agencies.
Researchers are actively investigating methods to streamline early intervention trial progress. They are concentrating on developing clinical endpoints by gathering feedback from patients and through anatomical and functional markers. To achieve this objective, experts have collaborated to form a consensus group to establish a more comprehensive grading of age-related macula severity that accounts for early biomarkers and surrogate endpoints.
Innovation in technology and strategies such as AI integration into screening tools, developing advanced home-based monitoring tools, and prioritizing marginalized and vulnerable groups show promise in the fight against age-related macular degeneration and other retinal disorders.
Effective therapies for macular degeneration have the potential to unlock a new era of transformative outcomes, significantly reducing the disease burden on aging populations. Investing in developing treatments for age-related macular degeneration can create far-reaching impacts that benefit millions globally.

