Stem Cell Therapies For Retinal Disorders Are A Sight For Sore Eyes
(Posted on Saturday, August 5, 2023)
Originally published on Forbes on 7/29/2023
This story is part of a series on the current progression in Regenerative Medicine. This piece is part of a series dedicated to the eye and improvements in restoring vision.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
Is it possible to restore vision with our cells? Can you believe that soon we may witness this reality in front of our eyes? Seeing may be believing, but this scientific breakthrough will allow us to believe in something we’ve never seen before.
With numbers like these, it’s no surprise there is an increasing focus on the potential of stem cell therapies to restore vision loss. In fact, at least ten different clinical trials currently look at stem cell therapies for vision loss. There are also a variety of preclinical studies underway, one of which we will look at in further detail in this piece.
Of the 2.2 billion cases of vision impairment, over one billion could have been prevented or are currently neglected. Digging deeper, at least eight million people face total blindness from age-related macular degeneration.
Age-related macular degeneration (AMD) is a degenerative disorder that affects the macula, the central part of the retina responsible for precise and detailed vision. It’s the foremost reason for irreversible vision loss in the aging population of developed countries, with advanced age-related macular degeneration affecting over 2 million people solely in the United States.
A diagram of a healthy macula, dry macular degeneration, and wet macular degeneration.ACCESS HEALTH INTERNATIONAL
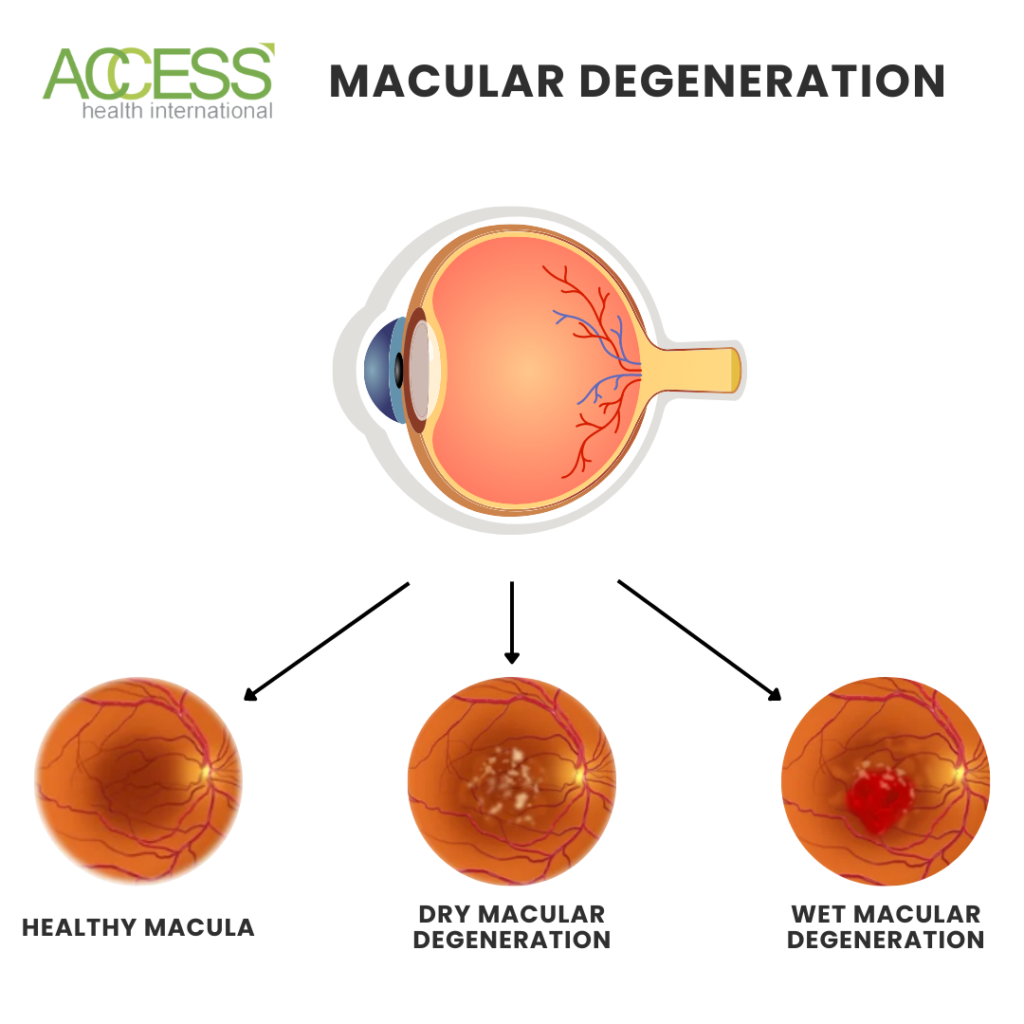
It has two major clinical presentations: dry and wet.
Dry age-related macular degeneration, which accounts for about 85 to 90% of cases, progresses slowly and is characterized by the accumulation of yellowish deposits called drusen in the macula. This accumulation eventually leads to the breakdown of the retinal layer called the retina pigment epithelium. It also disrupts blood vessels that are situated behind the retina. This disrupts normal cell metabolism, leading to the death of photoreceptor cells and, eventually, geographic atrophy, which causes irreversible vision loss.
Wet macular degeneration accounts for the remaining cases and is characterized by abnormal blood vessel growth that leaks blood and fluid into the macula. As blood leaks into the eye, it can cause a separation of the light-sensing photoreceptor cells from the retinal membrane. This separation prevents cells from receiving much-needed nutrients through the retinal membrane. A lack of nutrients can cause the photoreceptor cells to die, which leads to blindness.
Although there is no cure, various treatments are available to slow its progression and enhance the quality of life for patients affected by it. Treatment options for wet macular degeneration include anti-vascular endothelial growth factor (anti-VEGF) therapies that stop the growth of abnormal blood vessels and photodynamic therapy that uses laser and light-sensitive medication to destroy abnormal cells. Dry macular degeneration is more challenging to treat, with antioxidant and vitamin supplements showing only modest benefits. However, research into innovative therapies such as stem cell therapy, gene therapy, and implantable retinal devices offers hope for the future.
Stem Cells for Photoreceptors
Duke-NUS Medical School, the Singapore Eye Research Institute, and the Karolinska Institute do one such study. This preclinical study has produced significant vision recovery in a trial using stem cells to form light-detecting or photoreceptor cells in the eye.
In this study, the researchers introduced a human retina-specific protein called LN523 to cultivate human embryonic stem cells. This protein has been reported to be enriched in the retina and brain, suggesting that it might help to create an ideal retinal environment, facilitating the differentiation of pluripotent stem cells into photoreceptor cells.
The study results showed that introducing LN523 into the retinal matrix led to the differentiation of embryonic stem cells into photoreceptor progenitors within 32 days of culture. Furthermore, the researchers found that the embryonic stem cell-derived photoreceptor progenitor cells could engraft in the genetic retina degeneration rodent model and rabbits with a degenerated retina. This means these stem cells can live in mouse and rabbit retinal matrixes, allowing them to create more photoreceptor cells and replace those lost to degeneration.
The researchers used a retinal test called a full-field electroretinogram to investigate the functional recovery of the transplanted rodent retina. They found that short-term functional recovery was detected despite cell engraftment in a confined targeted host retina region. The transplanted human photoreceptor progenitors expressed mature markers and exhibited synaptic connectivity with the host’s inner retina after 3 to 5 months post-transplantation.
From Findings to the Future
These findings suggest that LN523 can be a promising approach for differentiating stem cells into photoreceptor progenitors for cell-based therapy in patients suffering from retinal degenerative diseases. The researchers plan to refine the protocol and test against cells in photoreceptor degeneration that are more closely related to the human eye. If practical, they hope to start clinical trials.
The study faced limitations, including the lack of a method to purify photoreceptor progenitor cells and the ability to perform cell transplantation in a fully depleted photoreceptor retina to demonstrate clinical applicability. Additionally, the full-field electroretinogram used in the study only detected short-term functional improvement post-transplantation.
Despite certain limitations, studying cell transcriptomic profiles and post-transplanted animal models showed partial improvement in vision and no teratoma growth. This indicates that the retina-specific laminin-based, LN523, photoreceptor differentiation method could be a safe avenue for treating retinal degenerative conditions.
While more work remains, this study presents a promising opportunity for sorting photoreceptor progenitor cells. Such advances could significantly improve functional retina outcomes after transplants, laying the groundwork for future discoveries in mechanistic pathways involved in the progression of macular degeneration. Ultimately, such progress may enable the discovery of alternative therapies for individuals suffering from retinal degenerative diseases.
To learn more about the eye, read more stories at www.williamhaseltine.com

