Bionic Breakthrough: The Future of Bioelectronic Prosthetics
(Posted on Wednesday, October 25, 2023)

SWNS
This article was originally published on Forbes on 10/25/23.
This story is part of a series on the current progression in Regenerative Medicine. This piece discusses advances in brain-machine interfaces.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
A new bionic hand demonstrates the advances made in brain-machine interfaces in recent years. Throughout my series on regenerative medicine, I have discussed a number of brain-machine interface innovations that display the modern era of regenerative bioelectronics. A field that has advanced rapidly in recent times is prosthetic technology, whether that be exoskeletons for neuromuscular patients or artificial skin.
Most recently, Dr. Max Ortiz-Catalan and colleagues from the Center for Bionics and Pain Research in Mölndal, Sweden, published their work in Science Robotics on a new-age bionic hand, among the most state-of-the-art seen today. Here, I will discuss their bionic hand and how it may impact regenerative prosthetics and the brain-machine interface field moving forward.
The Ortiz-Catalan bionic hand is far from the first brain-machine interface-enhanced prosthetic. In previous articles, I have discussed advances in haptic technologies to allow amputees to recreate the sensation of touch, as well as prosthetics that could move using brain impulses. How, then, is the Ortiz-Catalan hand any different?
There are three main aspects to demonstrate the hand’s sophistication: user integration, sensory feedback, and durability.
Most brain-machine interfaces are connected to the user via the nervous system, whether by integration to nerve endings in the limbs or spine or directly to the brain via an implanted chip. This enables the user to send and receive impulses, which can be used to control prosthetics and receive sensory feedback.
The Ortiz-Catalan hand takes integration a step further. In addition to the electrical connection between the hand and nervous system through a series of electrodes implanted in the patient’s arm, the prosthetic limb is also directly attached to the skeletal system by osseointegration.
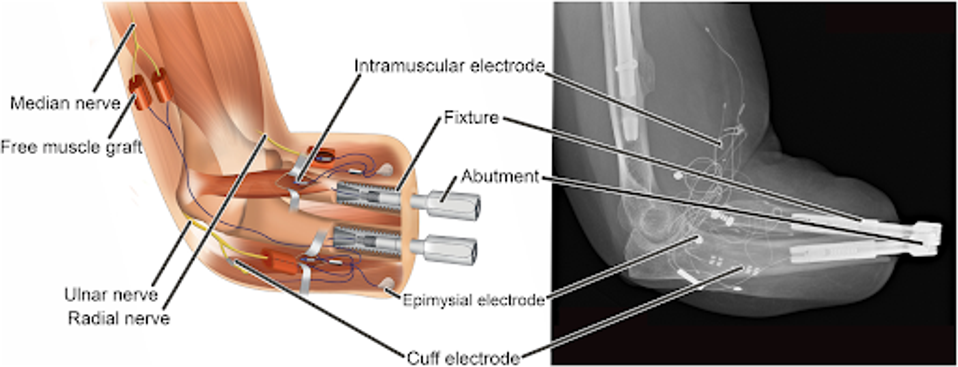
FIGURE 1: Schematic illustration and x-ray of a highly integrated human-machine interface in a patient with trans-radial amputation.
Among the most common complaints by prosthetic users is uncomfortability of the attached prosthetic. Ortiz-Catalan and colleagues found the affixed, osseointegrated prosthetic was far more comfortable for users on an extended-use basis.
Further, the unit is completely self-contained to the arm. Many brain-machine interfaces require clunky additional accessories to store batteries and processing units. Those items are stored in a small wristband attached to the wrist of the bionic hand, reducing the weight of the device and removing the cumbersome accessories.
In terms of functionality, the hand is also of the highest quality. Performing a series of daily living activities, such as packing a suitcase or cutting vegetables with a knife, a patient was tested pre-intervention, wherein the patient used a traditional prosthetic, and post-intervention with the Ortiz-Catalan hand.
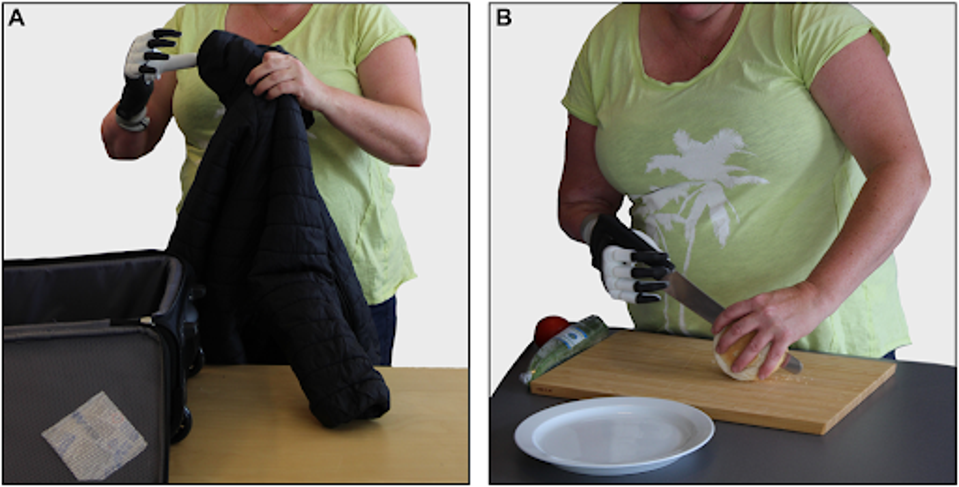
FIGURE 2: The patient performs tasks representative of daily life.
In both tasks, the patient improved between 13 and 23% as judged by the Assessment of Capacity for Myoelectric Control, indicating a significant increase in task efficiency. By another metric, the Southampton Hand Assessment Procedure, the patient improved again by 23% post-intervention.
The patient could also use the hand’s sensory installations to feel and describe the texture and shape of the objects they were holding, demonstrating the dexterity and sensory feedback of the bionic hand unit.
Durability is the third facet of the Ortiz-Catalan bionic hand. Over a period of several years, the monitored patient required intervention on the bionic hand only twice. The first was for a failed titanium support piece, and the second was for a failed screw. Both pieces were easily altered for improved stability and replaced. Neither the electrode wiring nor the osseointegration pieces failed or were impacted. The patient continues to wear and use the hand five years post-integration, demonstrating the unit’s long-term viability.
Of course, the great concern with advanced bioelectronics is cost. Similar high-end bionic hands have cost between $20,000 and $50,000 per device. Some more basic bionic hands begin around $1,000.
While the ultimate goal is to create regenerative technologies that are accessible to all who could benefit from them, the reality is that the complexity and novelty of these devices will price out many for the time being. As time rolls on, electronics will naturally become more affordable as the technology advances and becomes mainstream.
This is not to take away from the advances achieved by Ortiz-Catalan and colleagues. Their progress charts new ground as we continue to progress in the field of brain-machine interface regenerative bioelectronics. I eagerly await what others may have in store to follow this achievement.

