The Case For Safer Emergency Use Authorizations
(Posted on Wednesday, September 9, 2020)
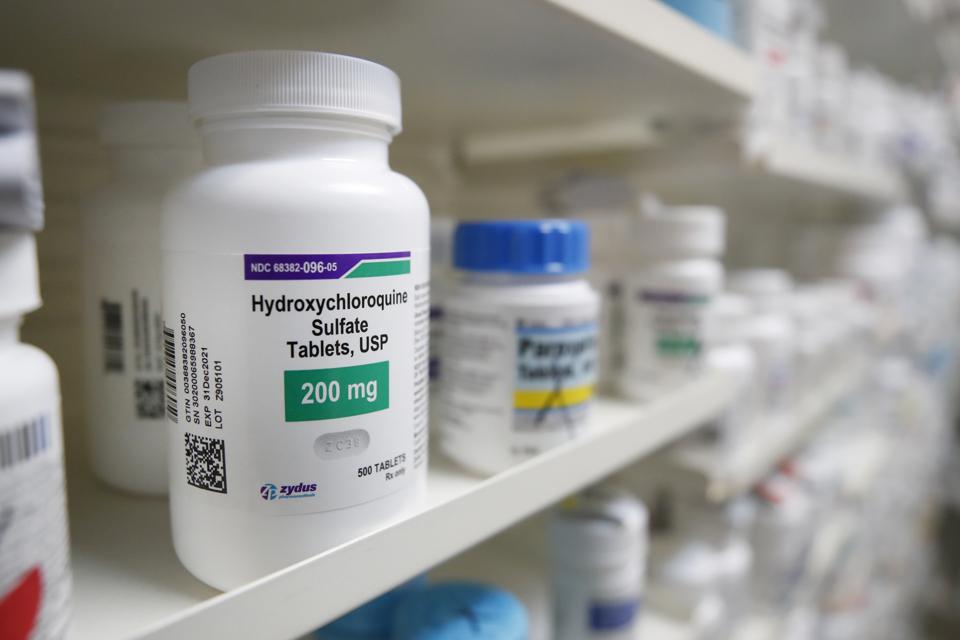
Hydroxychloroquine sits on a shelf at Rock Canyon Pharmacy in Provo, Utah, on May 20, 2020. – US President Donald Trump announced May 18 he has been taking hydroxychloroquine for almost two weeks as a preventative measure against COVID-19. (Photo by
AFP VIA GETTY IMAGES
In emergency situations such as Covid-19, emergency use authorizations (EUA) are vital and necessary. There needs to be effective treatments and vaccines available to stop the spread of this virus. The failures like hydroxychloroquine show that the EUA process must be robust enough that the authorized products do not harm the public or entrench public distrust of medicine. There cannot be EUAs for products that do not work.
The EUA for hydroxychloroquine and its eventual revocation show the shortfalls of the current EUA process. The treatment did not help Covid-19 patients and brought potential health risks to patients. Hydroxychloroquine should never have been authorized in the first place. The approval process must be revised for the safety of the population.
The Food and Drug Administration (FDA) authorized hydroxychloroquine on March 28th after being the current Administration lauded its supposed effectiveness. The authorization letter did not describe evidence that suggested hydroxychloroquine was a successful therapeutic. It only alluded to a limited French study of thirty six participants. Within a few months, the scientific consensus was that hydroxychloroquine was ineffective in reducing the symptoms of Covid-19. The FDA revoked hydroxychloroquine’s EUA on June 15th.
While “emergency use” implies haste, the quick process raises questions about the safety and effectiveness of a treatment. Understanding these treatments and their effects requires large studies over a significant amount of time. Pushing healthcare products without these studies is too much of a shot in the dark.
The FDA is under strong political pressure as well. In addition to the Administration’s push for new treatments, public pressure to approve therapies may move the FDA towards authorization even faster. The ideal world is one where the FDA approves EUAs solely on expert advice. Then the public sees the success of the expert backed EUA and continues to support the FDA.
An understated consequence of an EUA failure is the further erosion of trust in the healthcare system and its governing bodies. Federal bodies approving and revoking authorization for treatments in rapid succession will be noticed by the public. Trust in the medical field is low, so this unregulated cycle will exacerbate public skepticism and lower confidence in future potential vaccine approvals.
How can we improve the success rate of EUAs? First, authorization cannot move forward without examination and approval of an external advisory committee composed of independent experts, patients representatives, and other stakeholders. The advisory committee deliberations must be fully transparent, even live-streamed.
Second, the FDA must insist on post-marketing phase four surveillance of the drug or vaccine for safety in a much larger group of patients for a much longer period than required for the initial authorization. A product that fails to meet the safety and effectiveness standards in a phase four trial is denied. Additionally, emphasizing the National Vaccine Injury Compensation Program to the public will ensure that those skeptical of a drug or vaccine’s success will have the assurance of compensation in case something happens after a potential drug or vaccine is authorized.
Third, the FDA must work diligently to inform the public and communicate the criteria for approval, the data supporting any recommendation, the advantages and risks of the product, and the provisional nature of EUA. There is no such thing as too much communication between federal agencies and the public during a pandemic. The FDA must be as open as possible in their authorization of treatments.
These reforms would lead to an increased sense of transparency and accountability for the public, as well as a more robust approval process to ensure the safety and effectiveness of the authorized products. The consistent approval of successful EUA decisions would encourage the use of EUA treatments and that could potentially lead to an end to the pandemic sooner than otherwise.
Read original article on the Forbes website (published September 9, 2020)

