Hepatitis C, The Disease, Epidemiology, Treatment, Eradication Part 3: United States Epidemiology
(Posted on Tuesday, March 14, 2023)
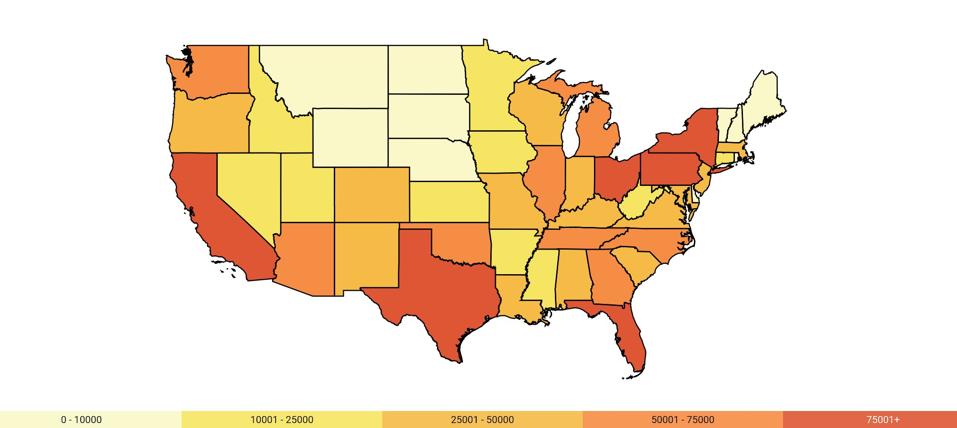
CONTINENTAL US MAP OF ESTIMATED NUMBER OF HEPATITIS C CASES FROM 2013-2016
HEPVU.ORG
Hepatitis C is the leading blood borne infection, and the number one cause of liver disease in the United States. The Center for Disease Control estimates that 2.7 million people in the US are currently living with a chronic Hepatitis C Virus infection with about 17,000 new chronic cases developing each year. The incidence of acute hepatitis C is equally concerning and has more than doubled since 2013. Though the national burden of hepatitis C presents an urgent public health emergency on its own, stratified data about its incidence, prevalence, and mortality show that the burden of hepatitis C varies by geographic and demographic groups. In this article, we’ll illustrate the scope of hepatitis C infections in the United States and highlight the inequities in disease burden across various groups of people.
Surveillance of Hepatitis C Virus in the United States
Epidemiological data on hepatitis C is dependent on data reported by individual health departments to the CDC. Since different states and jurisdictions have variable access to surveillance resources, estimates of incidence and prevalence are often greater than reported cases. In 2020, a total of 4,798 acute infections were reported to the CDC, but extrapolated estimates put the total number of acute infections to be around 66,700 cases. The CDC has instituted several strategies to address underreporting and promote more accurate data collection. CDC criteria of acute hepatitis C cases has become increasingly sensitive in recent years, and the specificity has enabled health departments to better catch cases that would not have been classified as hepatitis C in the past. Increasing testing efforts have also enabled smaller health departments to catch acute cases which are most often asymptomatic and less likely to be diagnosed.
Disease Burden by Geographic Region
The incidence of both acute and chronic hepatitis C infection varies by region of the United States. In 2019, the national rate of acute infection was 1.3 cases per 100,000 people. When stratified by state, however, the eastern and southeastern regions had the highest infection rates. In 2020, Maine had the highest incidence (11.9 cases per 100,000), followed by Florida (6.1 cases per 100,000), Louisiana (6.0 cases per 100,000), and West Virginia (5.3 cases per 100,000). In that same year, the states with the highest incidence of chronic hepatitis C were in West Virginia (122.1 cases per 100,000 population), followed by Alabama (115.8 cases per 100,000 population), Louisiana (90.6 cases per 100,000 population), and Mississippi (88.1 cases per 100,000 population). States that have been hit hardest by the opioid epidemic tend to have the highest rates of new infection, and as the opioid crisis continues to grow, those rates are rapidly increasing. From 2006 to 2012, acute hepatitis C infections increased by 364% in Kentucky, Tennessee, Virginia, and West Virginia. Incidence of both acute and chronic cases is also higher in rural regions, where public health resources are low, and treatment may be difficult to obtain.
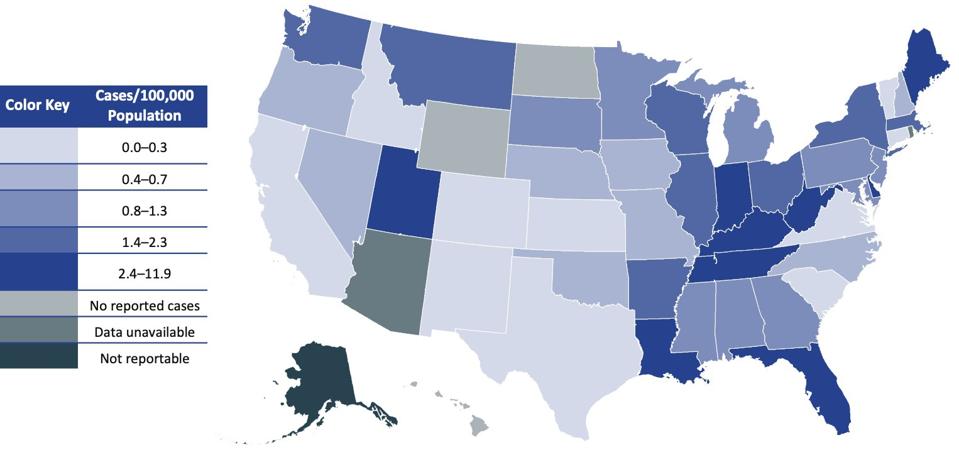
US MAP OF ACUTE HEPATITIS C VIRUS INFECTION INCIDENCES IN 2020. MAINE HAD THE HIGHEST RATE OF 11.9 NEW CASES PER 100,000 PEOPLE.
CENTER FOR DISEASE CONTROL
Disease Burden by Demographic Characteristics
Increased surveillance in the United States has also revealed demographic differences in hepatitis C epidemiology. Historically, males have had higher rates for chronic infection and of the 107,300 newly chronic cases reported in 2020, 64% occurred in males. In 2019, the incidence of acute hepatitis C infections was also slightly higher for males (1.6 new infections per 100,000) than females (1.0 new infections per 100,000).
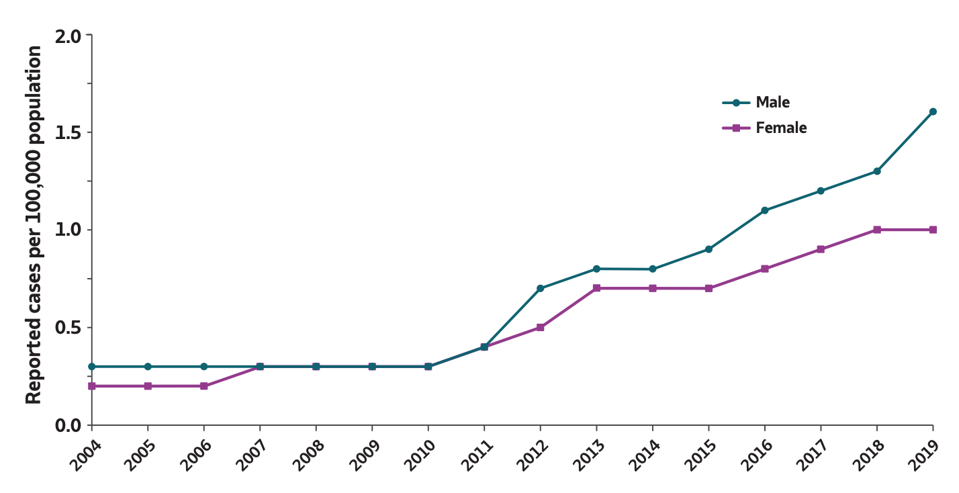
INCIDENCE OF ACUTE HEPATITIS C VIRUS INFECTIONS BY SEX FROM 2005 TO 2020. THE 2020 INCIDENCE OF ACUTE HEPATITIS C INFECTIONS WAS HIGHER FOR MALES (2.0 NEW INFECTIONS PER 100,000) THAN FEMALES (1.0 NEW INFECTIONS PER 100,000).
CENTER FOR DISEASE CONTROL
Baby boomers and millennials carry the most disease burden when compared to other age cohorts. Older generations have the highest prevalence with 75% of chronic cases appearing in persons born between 1945 and 1965, prompting many hospitals and healthcare institutions to implement mandatory Hepatitis C Virus testing for persons in that cohort. In 2019, both the reported number and rate of acute hepatitis C infections were highest among persons aged 20-29 and 30-39 years of age. It is important to note that the chronic infection prevalence among persons born between 1945 -1965 corresponds with the high incidence rate that occurred among young adults using intravenous drugs in the 1970s and 1980s. Similarly, the current spike in acute incidence rates among millennials aligns closely with the age cohort most affected by the opioid crisis. A greater focus on limiting transmission through injection drug use is, therefore, instrumental in addressing the rising incidence of acute cases in the United States.
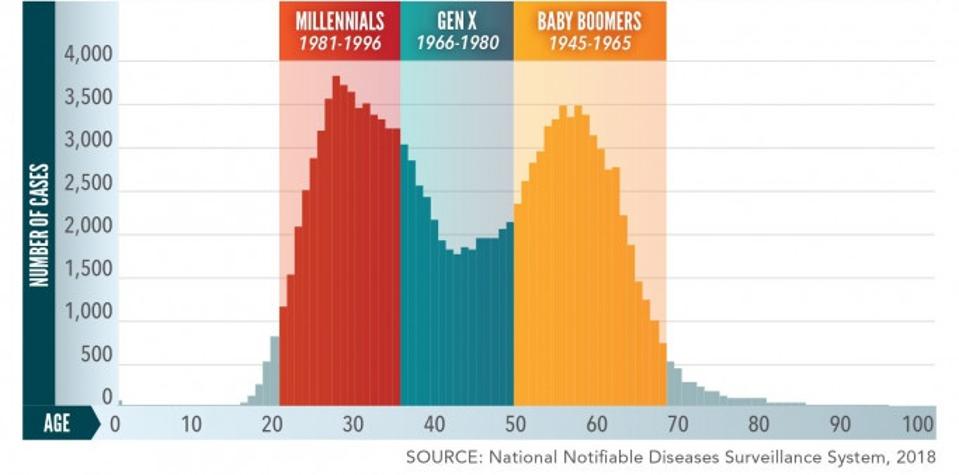
2018 HEPATITIS C PREVALENCE BY AGE COHORT. MILLENNIALS AND BABY BOOMERS HAVE THE HIGHEST NUMBERS OF INFECTION.
NATIONAL NOTIFIABLE DISEASE SURVEILLANCE SYSTEM
American Indian/Alaskan Native and non-Hispanic black communities are disproportionately affected by the Hepatitis C Virus. The incidence of acute infections in 2020 was highest among those of American Indian/Alaskan Native ethnicity (1.2 per 100,000) followed by white non-Hispanic (1.6 per 100,000), black non-Hispanic (1.1 per 100,000), Hispanic ethnicity (0.7 per 100,000), and Asian/Pacific Islander (0.4 per 100,000). Trend data collected from 2003 to 2019, shows a dramatic increase in the rate of reported acute infections among American Indian/Alaska Native individuals while data from 1999-2016 shows the highest hepatitis C prevalence among Black persons.
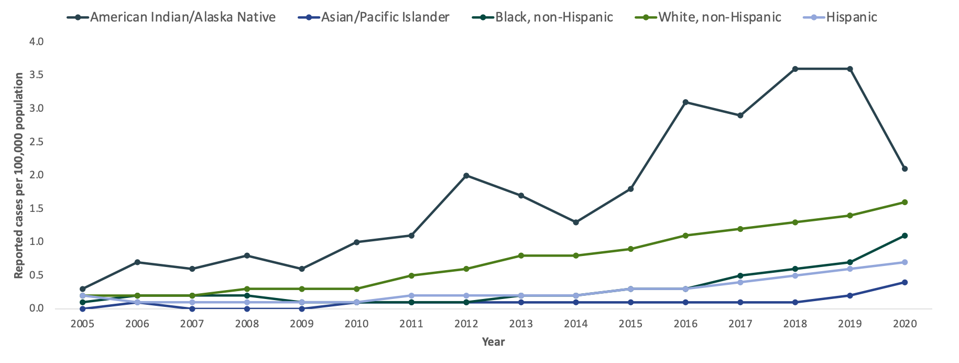
INCIDENCE OF ACUTE HEPATITIS C VIRUS INFECTIONS BY RACE/ETHNICITY FROM 2005 TO 2020. THE INCIDENCE OF ACUTE INFECTIONS IN 2020 WAS HIGHEST AMONG THOSE OF AMERICAN INDIAN/ALASKAN NATIVE ETHNICITY (1.2 PER 100,000).
CENTER FOR DISEASE CONTROL
Disease Burden Among the US Incarcerated Population
Although prisons and correctional facilities are required to treat and care for the medical needs of their populations, they are notable hotspots for Hepatitis C Virus transmission and mortality. Many incarcerated individuals are at high-risk for hepatitis C due to previous intravenous drug use and unsanitary tattoo needle use while incarcerated. It’s estimated that between 12% and 35% of people in prison have hepatitis C, a much larger percentage than the estimated 2% of the general US population. Without widespread testing and access to curative treatments, incarcerated individuals also carry a disproportionate mortality burden. In 2019, the hepatitis C-related death rate for incarcerated individuals was more than double the rate in the general population. These inequities require immediate attention to address preventative mortality and morbidity.
Morbidity and Mortality
In 2019, there were 15,000 hepatitis C related deaths in the United States—a mortality rate of 3.33 deaths per 100,000 people. Though this rate was a 32% decrease from the 2015 mortality rate, not all geographic and demographic groups have seen such a decline. States with the highest mortality rates in 2019 were Oklahoma and the District of Columbia (10.75 and 10.08 deaths per 100,000 respectively). California (2,114 deaths), Texas (1,383 deaths), and Florida (1,025 deaths) had the highest number of reported hepatitis C-associated deaths and accounted for more than 30% of all the hepatitis C related deaths reported in 2019. In 2020, the total number of hepatitis c-related deaths was highest in White persons (9,397 people), but death rates were highest among American Indian/Alaskan Native and non-Hispanic Black persons (10.17 per 100,000 and 5.63 times per 100,000, respectively). In fact, Hepatitis C Virus related chronic liver disease is currently the 5th leading cause of death among American Indian/Alaskan Native persons. Although men experience the highest burden of Hepatitis C related death, the rates are increasing disproportionately among women. From 2008 to 2012, the liver cancer-related death rate increased by an average 2.8% per year among men and 3.4% per year among women.
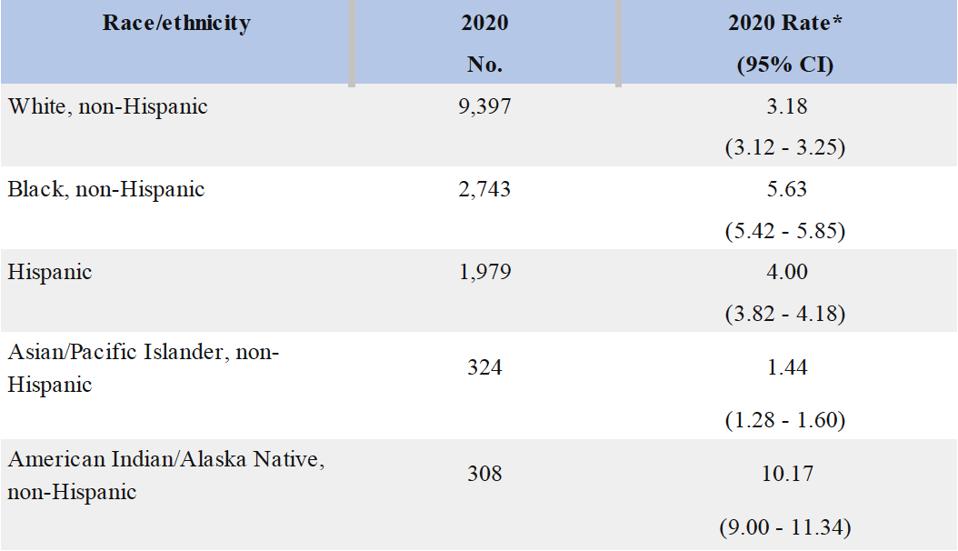
2020 HEPATITIS C-RELATED DEATH NUMBERS AND RATES BY RACE/ETHNICITY. *RATES ARE AGE-ADJUSTED PER 100,000 US STANDARD POPULATION DURING 2000
CENTER FOR DISEASE CONTROL
Although the United States has one of the more robust surveillance and health systems in the world, epidemiological data reveals striking inequities in hepatitis C burden. The lack of response to address the most vulnerable populations is just one roadblock to the eradication of hepatitis C in the United States. In the next part of this series, we will cover another roadblock to eradication—the inaccessibility of treatment for the Hepatitis C Virus.