Putting COVID-19 Behind Us: A Research Agenda To Prepare For The Next Pandemic
(Posted on Friday, May 8, 2020)
Though many today are too young to remember, this is not the first time our nation has faced down a lethal pandemic. Indeed, this is the third time in my life the world has been overwhelmed by contagions that reshaped societies. The first, polio, struck parts of Europe and North America well before I was born and plagued countries for more than half a century before scientists discovered a vaccine. The second, HIV/AIDS, hit when I was an adult and when I was thankfully better placed to be an active part of the team of scientists and public health leaders working on our response.
This third pandemic hit just as hard as the previous two — though it shouldn’t have. Unlike the others, we knew well in advance this one was coming. In the midst of two previous coronavirus outbreaks, SARS and MERS, scientists scrambling to find a medical solution warned us to prepare for the inevitability of another deadly outbreak of the virus. They started work on a number of promising drugs, some of which could act not just against a single strain of coronavirus, like MERS, but against the whole family of coronaviruses including today’s SARS-CoV-2.
But once the SARS and MERS outbreaks were over, interest in developing these drugs all but disappeared. Pharmaceutical companies lost interest, governments forgot about the scientists’ warnings, and the rest of us went about our regular lives, having never had to face our worst fears.
Someday — soon I hope — this outbreak too will be behind us. With an effective vaccine or treatment for COVID-19 in hand, we will, once again, return to daily life. And perhaps, just as we did after previous pandemics, we will begin to believe that the worst is behind us. But we will be wrong.
There is a whole world of other biological threats lying in wait, more deadly and more transmissible than today’s SARS-CoV-2. These looming biothreats are far from unknown. In 2015, the World Health Organization began prioritizing diseases that posed a threat to global health. By highlighting the diseases with the greatest risk, the thinking was that researchers and drug developers could prioritize efforts to tackle a solution. Among the diseases currently on the WHO list are SARS, MERS, and COVID-19, alongside other diseases of global renown, like Ebola and Zika.
But there are many other threats beyond that list alone. Think of viruses as nature’s own form of artificial intelligence, constantly learning and adapting to find the best way to exploit their environment. Humans have created a rich environment indeed. In the last hundred years, our population has more than quadrupled, with many of us living and working in high density urban clusters where viruses can easily spread and thrive. Fold in our increasingly global way of life and you have the recipe for successive pandemics that will engulf us with more frequency than in the past.
Our awareness of the threat of anew pandemic has become so widely acknowledged that Hollywood has even jumped on board, with movies like Contagion which essentially tells the story of what we are living today. The difference is that in Contagion, the virus killed 2.5 million. Today, we are not yet near those numbers, but that’s not to say the next virus won’t be deadlier. Whether it takes the form of a new coronavirus outbreak, a more dangerous strain of influenza, or a new germ that is resistant to all available antimicrobial drugs, it will be devastating — more devastating than anything we are witnessing today.
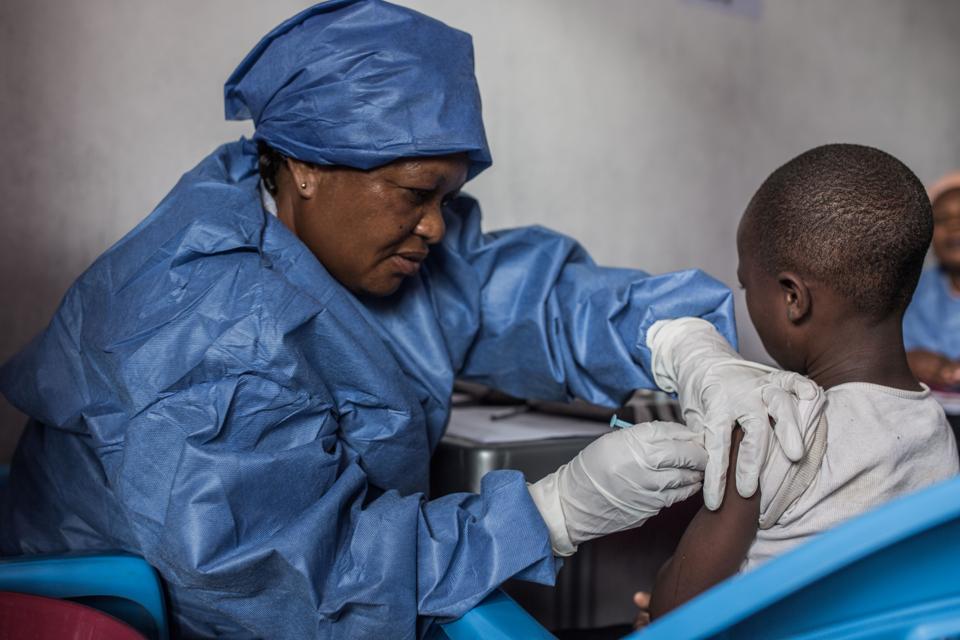
A girl is getting inoculated with an Ebola vaccine on November 22, 2019 in Goma. (Photo by PAMELA TULIZO / AFP) (Photo by PAMELA TULIZO/AFP via Getty Images)
AFP VIA GETTY IMAGES
Faced with the prospect of a whole host of potential pandemics, scientists have long advocated for the development of a global arsenal of panviral drugs — drugs that would work broadly across an entire family of viruses or even across multiple virus families instead of acting against a single disease.
The oral polio vaccine of today, for example, works only against two of the three types of polioviruses we know of — WPV1 and WPV3. Introduce WPV2 — an eradicated strain — into the mix and the vaccine has no effect. Panviral drugs wouldn’t have the same problem. Instead of helping the body develop immunity against a disease caused by a particular virus, a panviral drug attacks the virus itself, preventing it from replicating or performing key functions. Simply put, If you understand the overall structure of a family of viruses and how they work, you can start targeting elements of their architecture and destroy their ability to function.
The challenge is that developing a drug that targets a virus’ structure and processes is risky business. Any drug that works well at damaging the way an invading virus functions may also work far too well against the functioning of our own body’s cells. Creating safe and effective panvirals is a time-consuming and laborious process that takes years — sometimes decades — before bearing any fruit. So while we may have the knowledge and tools to develop these drugs as part of a pandemic preparedness watches, no scientist or laboratory has been given the time, the funding, and resources to take on the task.
The lack of resources dedicated to this effort by major pharmaceutical companies and the private sector is somewhat understandable, though perhaps not endorsed. If we could accurately predict that a hemorrhagic fever-causing arenavirus would sweep the globe in 2025, killing tens of millions, every pharmaceutical company in the world would focus their efforts on an anti-arenavirus drug, knowing there was a market in place should they prove successful. But without knowing what the next pandemic will be or when it will hit, no company would sign up for the effort in advance.
The onus then falls on governments to step in to fill the gap. Some governments have acknowledged the threat enough to create the programs that could now step in to help. The United States, for example, created the Biomedical Advanced Research and Development Authority (BARDA) in 2006. BARDA presides over the discovery, development, and stockpiling of medical countermeasures that protect Americans against health security threats. This includes biological agents of warfare, like anthrax, but also new and emerging infectious diseases, like the coronavirus.
BARDA has a substantial $1.5 billion budget, split into three distinct areas: advanced research and development on emerging infectious diseases, pandemic influenza, and antimicrobial resistance; Project BioShield, a biodefense program to prepare for a bioterrorist attack; and a domestic influenza preparedness program. It’s potential is huge, but its funds are poorly targeted. With the abrupt firing of longtime director Rick Bright, its effectiveness is called into even greater question.
In the absence of private sector or government leadership, new global partnerships among public, private, nonprofit organizations and by scientists themselves have taken root. The Coalition for Epidemic Preparedness Innovation was established in 2017 with substantial support from the Bill & Melinda Gates Foundation and the UK based Wellcome Trust, along with support from some major pharmaceutical players like GlaxoSmithKline. Their goal is to accelerate the development of vaccines against emerging infectious diseases and enable access to vaccines for all people in need during outbreaks. The Coalition represents exactly the kind of forward thinking research agenda that is needed to prepare us for the next pandemic. Yet, to date, only seven countries and the European Commission have committed ongoing funding for their work.
Meanwhile, scientists at the Structural Genomics Consortium (SGC), the University of North Carolina at Chapel Hill and the Eshelman Institute for Innovation, recently announced a new initiative — the Rapidly Emerging Antiviral Drug Development Initiative (READDI) — which is raising $125 million to generate five new drugs in five years to ready our world for the next pandemic.
These efforts are still not enough to prepare us entirely, but they are an important start. We should count ourselves lucky that SARS-CoV-2 is not more deadly. We cannot forget — the bubonic plague killed 400 million, the 1918 flu killed 50 million, and the HIV/AIDS epidemic has killed more than 35 million, with numbers still rising. We may like to think we’ve gotten smarter and stronger since these outbreaks occurred — but for every advancement we have made, Nature has been right in step to match us. Let us not forget the warning she is giving us today.
This post originally appeared on Forbes (May 8, 2020).